Advances in high-resolution Nuclear Magnetic Resonance (NMR) spectroscopy are reshaping how we understand and detect inflammation in the body. Instead of relying on traditional, broad-strokes markers, clinicians and scientists now have access to a technology that provides a detailed snapshot of our immune activity, enabling them to distinguish acute from chronic inflammation with remarkable precision.
NMR Markers: A New Era of Inflammatory Insight
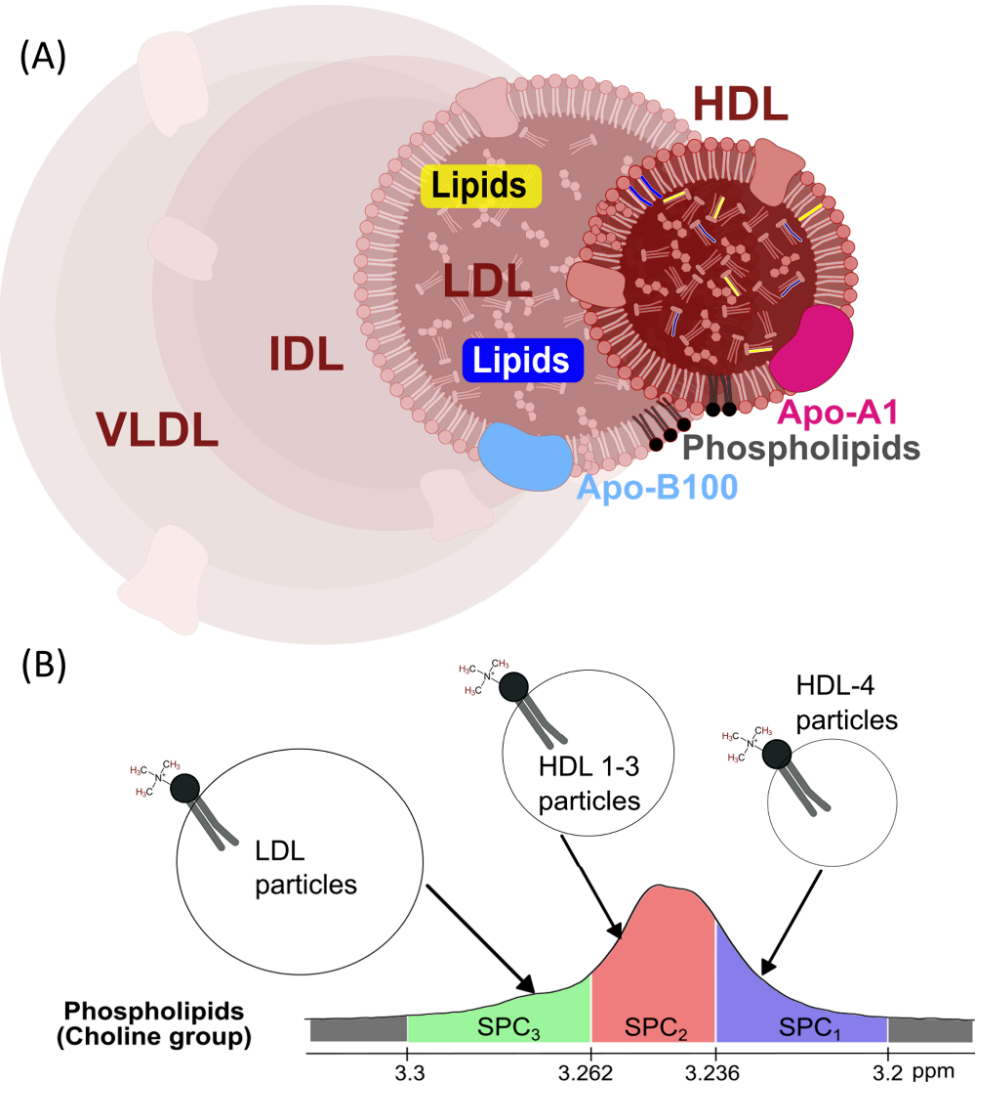
- Precise Inflammatory Signatures: NMR spectroscopy measures specific blood signals, namely, glycoproteins (GlycA, GlycB) and supramolecular phospholipid composites (SPC), yielding more nuanced information about the type and severity of inflammation than classic markers like C-reactive protein (CRP).
- SPC Subregions Uncover Disease Dynamics:
- In chronic inflammation (such as heart disease and diabetes), SPC2 and SPC3 levels drop, while SPC1 remains stable.
- During acute inflammation (as seen in sepsis or severe infections), SPC1 decreases, indicating severity, while SPC2 and SPC3 deviate from healthy baselines.
- Cardiovascular Risk Indicator: The SPC3/SPC2 ratio dramatically increases in both chronic and acute inflammatory states, closely paralleling the well-known apolipoprotein B100/A1 (ABA1) ratio and signaling potential risk for atherosclerosis.
- Distinct Biological Roles: Each SPC subregion offers unique diagnostic value, challenging the one-size-fits-all approach of aggregating SPC measurements.
- Accessible and Scalable: These markers can be measured using benchtop NMR devices, making advanced inflammation profiling feasible in routine clinical settings.
Figure 1. (A) Overview of the blood lipoproteins. Very low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), and the two subfractions visible using the DIRE experiment, the low-density lipoprotein (LDL) and high-density lipoprotein (HDL). (B) The segments of the composite SPC peak, SPC1, SPC2, and SPC3 in the DIRE NMR spectrum with the associated lipoprotein subfractions from which the peak arises from shown. Credit: Paper
Why Differentiating Inflammation Types Matters
Inflammation protects us from infections, but chronic, unresolved inflammation is a root cause of many diseases including stroke, cancer, and diabetes. Knowing whether a patient faces an acute immune flare-up or a lingering, damaging process is crucial for targeted treatment and risk prediction.
Traditional tests such as CRP, ESR, and procalcitonin often miss these subtleties. NMR-based markers, particularly the SPC subregions, give a more dynamic and comprehensive view of the inflammatory process and its metabolic effects.
Large-Scale Study: What the Data Revealed
Researchers examined over 5,700 blood samples from a wide range of people: those with chronic illnesses, COVID-19, and severe acute conditions in intensive care. Using specialized NMR techniques, they measured GlycA, GlycB, and three SPC subregions.
- Chronic inflammation showed a drop in SPC2 and SPC3, with SPC1 unchanged.
- Acute inflammation led to a notable decrease in SPC1, a pattern common in ICU patients with severe illness.
- The SPC3/SPC2 ratio stood out as a reliable marker for cardiovascular risk, distinguishing at-risk individuals from healthy controls.
- GlycA and GlycB both rose during inflammation, but each correlated differently with CRP, suggesting they capture unique facets of immune activity and metabolism.
- Importantly, none of the five markers varied significantly with age alone, indicating that elevated levels signal true disease rather than normal aging.
The Promise for Clinical Practice
Thanks to the ability of SPC subregions to differentiate between acute and chronic inflammation, clinicians could soon diagnose not only the presence of inflammation but also its type and severity. The SPC3/SPC2 ratio offers a valuable, non-invasive tool for assessing cardiovascular risk potentially transforming how we predict and manage heart disease.
With benchtop NMR technology now within reach for many clinics, these advanced tests could soon become a standard part of patient care, overcoming the cost and complexity of older, high-field NMR systems.
Toward Tailored Inflammation Assessment
This research signals a new chapter in how we understand and manage inflammation. High-resolution NMR biomarkers, especially the distinct SPC subregions, add a layer of precision that traditional tests simply cannot match. As these tools become more widespread, personalized diagnostics and targeted treatments for inflammatory diseases are set to become the new standard in medicine.

NMR Spectroscopy Is Transforming Inflammation Diagnostics
NMR Spectroscopy-Based Lipoprotein and Glycoprotein Biomarkers Differentiate Acute and Chronic Inflammation in Diverse Healthy and Disease Population Cohorts